AS PART OF HACKENSACK MERIDIAN HEALTH’S ONGOING INVESTMENT IN THE TREATMENT OF MOVEMENT DISORDERS, JFK JOHNSON REHABILITATION INSTITUTE IS OFFERING A BREADTH OF INNOVATIVE INPATIENT AND OUTPATIENT INITIATIVES TO FOSTER THE PHYSICAL, NEUROLOGICAL, AND EMOTIONAL WELL-BEING OF PARKINSON’S PATIENTS
BY AMANDA MCCOY • PHOTOS BY AMESSE PHOTOGRAPHY

According to data from the Parkinson’s Foundation, nearly one million Americans are currently living with Parkinson’s disease, with 90,000 new diagnoses each year. As a disorder of the central nervous system and neurotransmitter transmission, it often causes unintended or uncontrollable movements (tremors of the hands, arms, legs, and jaw are the most notable) along with muscle stiffness, impaired balance, hyportension, vocal changes, and more. It is progressive in nature, a lifelong disease, but a patient’s journey does not end with a positive diagnosis. There are paths for moderating an individual’s symptoms, therefore greatly improving their quality of life. Hackensack Meridian Health is actively expanding its Parkinson’s Disease and Movement Disorders Program across the entire network to provide comprehensive, individualized care and support for people living with Parkinson’s and their care partners, inside the hospital walls and out.
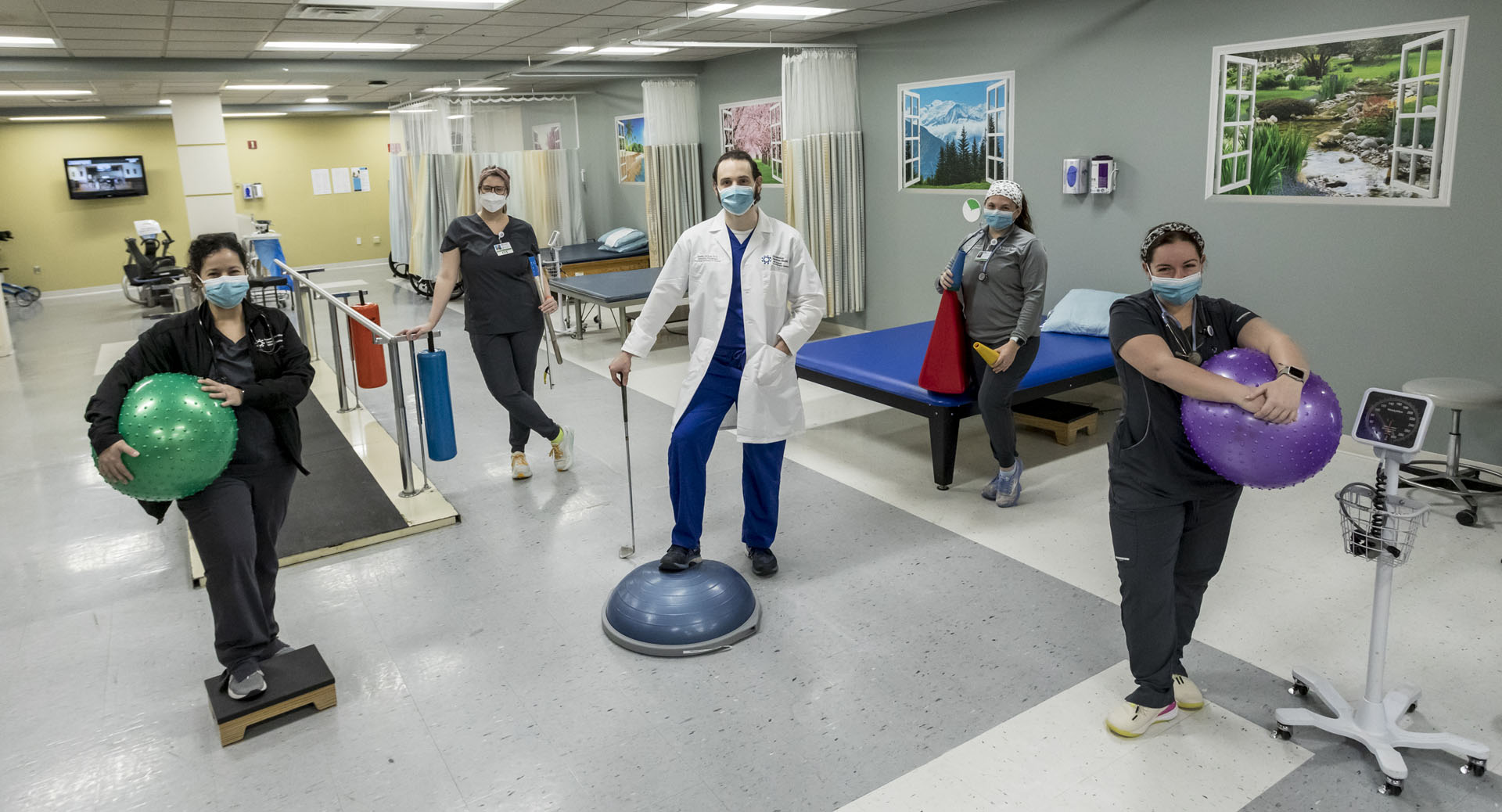
One area where HMH is significantly forwarding the future of care for Parkinson’s patients is through innovative inpatient and outpatient programs at JFK Johnson Rehabilitation Institute, a highly decorated Edison facility that is nationally ranked as a Top Rehabilitation Hospital in the Country by U.S. News & World Report. Here, a team of physicians, movement disorder specialists, and physiatrists, psychologists, therapists (PT, OT, ST), social workers, nutritional counselors, and nurses work together to address the full scope of physical, neurological, psychological, occupational, and emotional needs of individuals with Parkinson’s disease.
“All therapies work in synergy,” noted Roger Rossi, DO, a board-certified physiatrist with JFK and medical director of St. Joseph’s Wayne Medical Center, Acute Rehabilitation Unit in Wayne, who has extensively studied the neurological effects of Parkinson’s disease on movement, cognition, gait, posture, and speech patterns. “If you are undergoing one discipline without the other, you won’t experience as much improvement.”

According to Dr. Rossi, the three most common areas of therapeutic discipline include occupational therapy, which spans hygiene, fall prevention, activities of daily living, self-care, transfers, bed mobility strength, and balance, as well as adaptive equipment; speech therapy, which includes cognition, memory, swallowing, facial and vocal inflection, and vocal enhancement; and physical therapy, which stresses gait, posture, balance, core stability, and general ambulation and strengthening. “Parkinson’s patients also tend to have a high incidence of difficulties with sleep, associated depression, and apathy,” explained Dr. Rossi. “Psychological services as well as care provider reassurance and counseling is very helpful. People are often worried about their progression and how it will affect their families, work, activities, and care partners.”

Last year, the hospital launched the Parkinson’s Wellness Program, a two-week inpatient bootcamp for patients with Parkinson’s or Parkinsonism (individuals with Parkinson-like symptoms, often caused by multiple strokes or head traumas, as well as conditions such as PSP and MSA) who have recently suffered a setback or require significant medical attention.
“The wellness program is for patients who have experienced a deterioration in their progress or progression of their disease,” said Dr. Rossi. “The setback could be caused by anything from frequent falls, debility associated with a recent hospitalization, a urinary tract infection, or pneumonia that has compromised their condition.”
Dr. Rossi explained the program is highly tailored to the individual. After the patient is carefully evaluated across multiple disciplines, a custom treatment plan is created for the next two weeks to target their specific needs.

“To my knowledge we are the only rehab hospital in the country offering an inpatient rehabilitation program like this,” noted Steven Markos, MD, a board-certified physiatrist at JFK Johnson Rehabilitation Institute and medical director of JFK-JRI’s Parkinson’s Wellness Program. “We’re seeing tremendous improvements from both a medical and functional standpoint. We’re increasing a patient’s level of indepen- dence and endurance. When a patient develops a symptom like hypotension, it can limit their ability to stand up. We’ve seen patients progress from passing out nearly every day to walking without issues.”
When the program is complete, physicians use a series of quantifiable measures to ensure a safe discharge back into the community, assessing areas like motor activity, balance, visual-spatial awareness, and emotional well-being. But JFK’s support doesn’t end once the patient exits the facility.
“When a patient is discharged from the program, they have a very detailed strategy for continuation of the benefits they’ve achieved through a structured outpatient and community-based plan,” added Dr. Rossi.

Patients with Parkinson’s in New Jersey have access to a wealth of outpatient programs, community-based programs, and support groups that provide not only access to a community and a sense of inclusion, but foster activities that are medically proven to help manage symptoms. “Exercise and movement have been shown to prevent disease progression, decrease medications, control symptoms, enhance quality of sleep, and prolong the onset of symptoms,” said Dr. Rossi. “It’s just as valuable as medication.”
Rock Steady, for example, is a non-contact boxing program that focuses on weight shifting and range of motion to improve balance and coordination. It is a component of the PWR! Program, which was designed to amplify movement through fitness classes like yoga (for flexibility and balance), Tai Chi (for movement control), dance (for balance, coordination, and movement control), and BIG for LIFE to promote strength, balance, and voice modulation.
“These programs are beneficial because Parkinson’s patients in general may not perceive their postural limita- tions and movement patterns,” continued Dr. Rossi. “They are doing everything in a diminished fashion. Their voice is low, they might have decreased arm swing, narrow-based posture, and decreased stride length, so these programs work on amplification of movement. They encourage people to do everything with power, to do things bigger and louder.” Music is also a powerful healer and synergistic tool, noted both physicians. The Loud Crowd is a local vocal group that gathers virtually and in person to sing. They recently performed with a symphony in Red Bank. This group was developed as a community spin-off for individu- als who had received structure vocal training from speech and language pathologists. It benefits patients and their care partners by enhancing vocal quality, cognition, and facial expression, as well as serves as a method of socialization and engagement.
“The community aspect is so important,” added Dr. Markos. “A patient will always value their physician and therapists, but it resonates differently when they feel part of a community and can take part in a shared experience and perspective.”
