INSIDE HACKENSACK MERIDIAN HEALTH’S SPECIALIZED CLINIC, OFFERING ADDITIONAL CARE FOR PATIENTS SUFFERING FROM COVID 19’S LONG TERM EFFECTS
BY JESSICA JONES GORMAN • PHOTOS BY AMESSE PHOTOGRAPHY
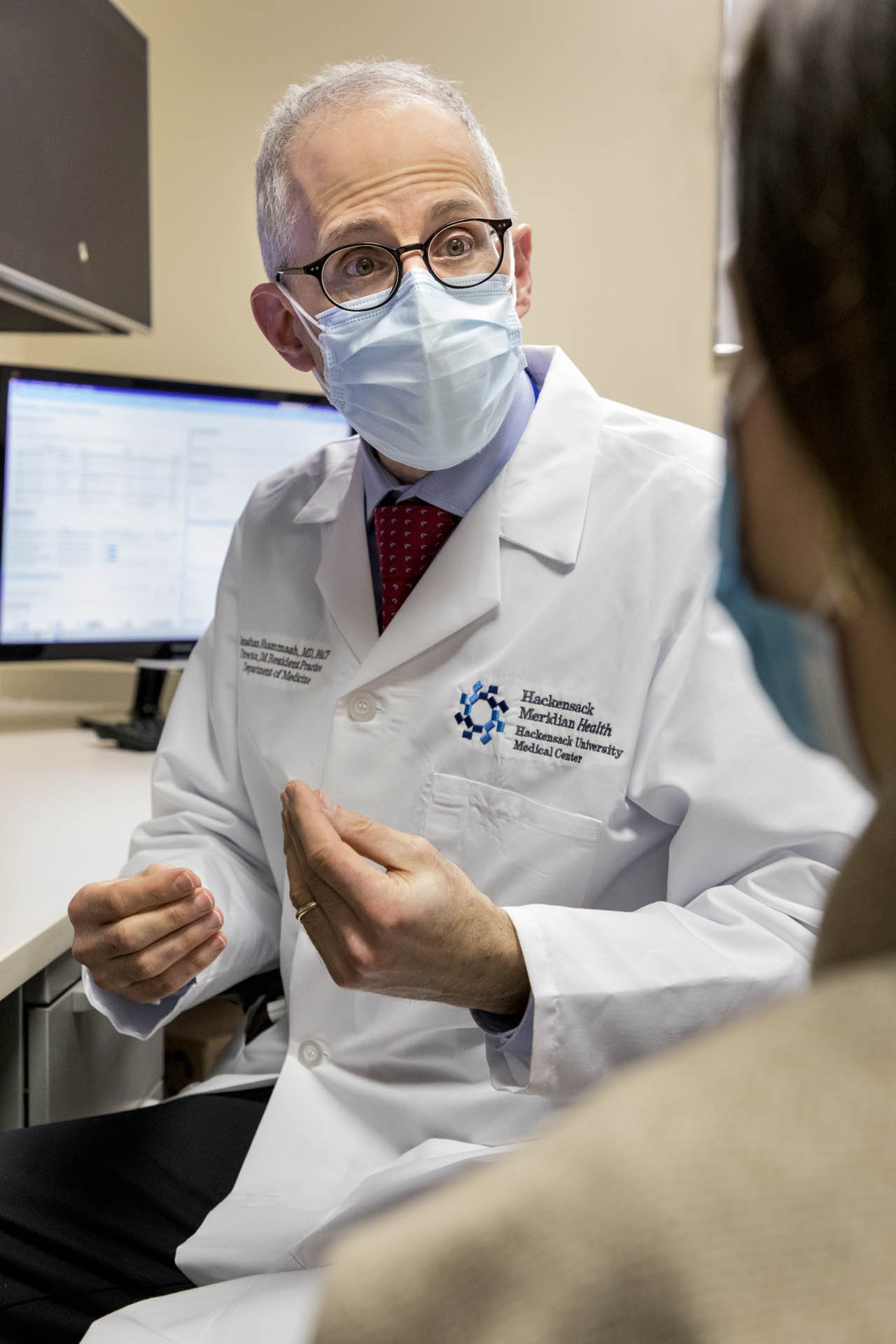
Hackensack Meridian Health has treated more COVID-19 patients in the state of New Jersey than any other hospital system, caring for more than 21,000 affected patients over the past year. They have identified the reality that many COVID-19 patients require additional care as they recover from the virus’ long term effects. To assist in that recovery, the healthcare network launched New Jersey’s first COVID-19 Recovery Center in July 2020.

“Research and innovation is part of HMH’s DNA, and this unique COVID-19 clinic is enabling HMH to gain valuable insight into the persistent symptoms that are sometimes experienced by patients who had infections with this virus,” noted Laurie G. Jacobs, M.D., chairperson of the Department of Internal Medicine at Hackensack Meridian School of Medicine and Hackensack University Medical Center. “This Recovery Center is helping COVID-19 patients across New Jersey and throughout the country as well.”
Treating more than 500 patients during the first six months of its operation, HMH’s COVID-19 Recovery Center focuses on a population of patients who continue to face lingering symptoms after diagnosis and treatment of COVID 19. Providing continued care to patients experiencing fatigue, shortness of breath, and other symptoms involving the lungs, heart, brain, and other parts of the body, the Center provides important medical support to those who need additional care, with the hope of providing new treatments.
“New Jersey has been one of the hardest hit states,” said Dr. Jacobs. “Investigating these chronic symptoms here is an important step in helping the residents of this state recover and rebound from this virus.”
Dr. Jacobs, who maintains a specialty in geriatric medicine, has been with HMH for more than four years. When the pandemic hit in March of 2020 her responsibilities expanded to ascertain physician staffing for the hospital and ambulatory care sites for COVID-19 cases. When the initial surge of the virus subsided in May, she embarked on a study with her colleagues to research how patients were faring a month after discharge.

“Research and innova tion is part of HMH’s DNA.”
“We began hearing that a number of patients were having continued symptoms 35 days or more after hospitalization,” she said. “Many complained of persistent symptoms that were impairing their quality of life and the ability to complete daily functions. Returning to work and performing ordinary tasks were problematic.”
So HMH decided to take a more in depth look at how and why these continued symptoms were occurring. While offering clinical care to patients with these side effects, doctors began compiling their health information to better understand why indications of their COVID-19 illness seemed to be lingering.
“More and more individuals started seeking our help, presenting with post COVID symptoms throughout the fall,” said Dr. Jacobs. “Our work started garnering national and then worldwide recognition as news of the network’s Recovery Center started circulating.”
In November Dr. Jacobs presented some of her team’s findings to the Social Security Administration since many symptomatic patients qualified for work related disability. She con curred with the findings of a nationwide discussion of symptoms and syndromes hosted by the National Institutes of Health in December, and the recent World Health Organization’s symposium on the topic.
Collectively referred to as “long haulers, by the public,” this syndrome has been renamed “post-acute sequelae of COVID19, or PASC” by the NIH. Those affected by this post COVID condition experience a myriad of signs and symptoms. Fatigue, shortness of breath, chest pain, lingering cough, fever, aches, and neurological complexities like insomnia, headaches, anxiety, depression, and brain fog are the most prevalent markers.
“The patients we’ve seen are so tired they cannot perform daily tasks and their minds are often so clouded they cannot think clearly or complete executive functions such as balancing a checkbook,” said Dr. Jacobs. “They are impaired in different ways but we all believe that there’s one unifying physiological cause manifesting itself in different parts of the body.”
This is by no means a new medical anomaly, the doctor explained. In fact, it’s a pattern that’s surfaced after other viral infections like Zika and Ebola; even certain strains of influenza and the bacterial illness Lyme disease have caused similar chronic ailments. HMH is committed to researching why a portion of COVID patients is currently experiencing the same problem.
“It’s not very clear who is at risk for these chronic symptoms,” noted the doctor. “This is occurring in patients who have been hospitalized and also in patients who have only experienced mild COVID symptoms. Some currently experiencing chronic fatigue were never aware they had COVID in the first place but the antibodies were present in their blood.”
Dr. Jacobs explained it’s important to note that most people who are diagnosed with COVID recover fully, and this condition affects only about two to ten percent of those who test positive. But those numbers still add up.
“Ten percent may not sound like a lot but when you consider how many people have been afflicted by COVID it’s a generous number,” she said. “The ‘why’ of this chronic problem is still poorly understood at this point, and doctors from all around the world are putting their heads together to figure out a cause for this and identify who is at risk. Most of us feel the virus initiated some kind of immunological response our center is focused on pinpointing why.”
HMH’s Recovery Center features a staff of primary care physicians, cardiologists, and pulmonologists working in conjunction with a team of neurologists, physical therapists, and other specialists to try to alleviate patient symptoms.
“Our cardiologists are looking at symptoms like palpitations and dizziness, and the pulmonologists are studying breathing issues and why they’re occurring,” said Dr. Jacobs.
“I’m very hopeful about the work we’ve done thus far. I believe we are moving forward in a very positive direction.”
“Not only are we treating these symptoms and attempting to alleviate them, we’re also deciphering the reasons behind them.”
The doctors in the program compare notes once a week and cooperatively analyze all of the latest data, weighing in and expressing ideas about any new therapies. According to Dr. Jacobs it’s that collaboration coupled with national and worldwide recognition of this condition that will help determine a cause and solution.

“The first step is to figure out who has it and why they differ from one another,” she concluded. “When we can figure out what predisposes it and how we can treat it. It’s too premature to make projections about the future, especially since this is a brand new disease. But I’m very hopeful about the work we’ve done thus far. I believe we are moving forward in a very positive direction.”
Hackensak Meridian Health COVID Recovery Center
hackensackmeridianhealth.org/COVIDcenter
