IN HONOR OF BACK-TO-BACK OVARIAN AND BREAST CANCER AWARENESS MONTHS, HACKENSACK UNIVERSITY MEDICAL CENTER’S CO-CHIEF OF ONCOLOGY DISCUSSES HOW THE FEMALE-LED ONCOLOGY TEAM IS COMMITTED TO CARE THROUGH COMPASSION, CLINICAL RESEARCH, AND CUTTING-EDGE INNOVATION
BY AMANDA MCCOY • PHOTOS BY AMESSE PHOTOGRAPHY
Of the five types of gynecologic cancers, ovarian cancer is the second most common, with approximately 20,000 new diagnoses each year, according to the Centers for Disease Control and Prevention. Though less prevalent than uterine cancer (which plagues an estimated 66,000 women every year), ovarian cancer claims more lives than any other cancer of the female reproductive system.

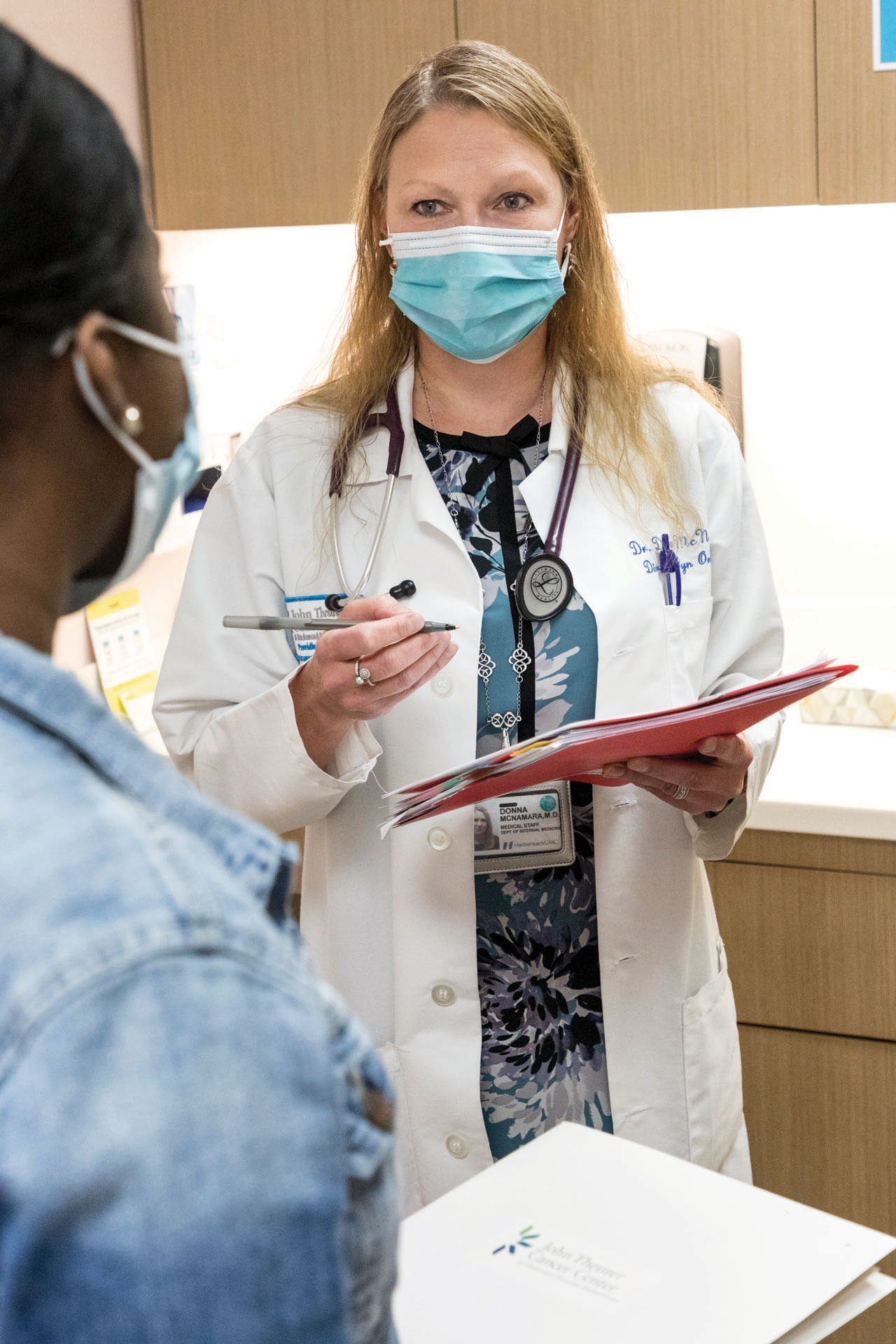
“Ovarian cancer is difficult to detect because the symptoms are so vague,” explained Donna McNamara, a medical oncologist and co-chief of gynecological oncology at the John Theurer Cancer Center at Hackensack University Medical Center (HUMC). “Many of the symptoms of ovarian cancer can be attributed to benign digestive issues, like a stomach ache, abdominal discomfort, gassiness, bloating, and changes in urination,” she continued. “Most patients see a gastrologist before learning this is a gynecologic condition. For that reason, most ovarian cancers are diagnosed in the later stages.”
Dr. McNamara treats a wide variety of female cancers, including ovarian, fallopian tube, uterine, cervical, and breast. She and her team are steadfast in their pursuit of advancing the care of women’s oncology services across the Hackensack Meridian Health (HMH) network, from implementing the latest in clinical technology to participating in novel clinical trials. When screening for breast cancer, for example, oncologists at HMH often administer an ultrasound in combination with a mammogram, which can significantly improve breast cancer detection in women with dense breast tissue. Dr. McNamara said there are also several advances underway in imaging that can better define the breast tissue – and as a bonus, many women find it to be less uncomfortable than traditional 2-D mammograms.
“The technology continues to evolve,” she said. “A 3-D mammogram, called tomo synthesis, can better define the breast tissue, and therefore is able to better delineate an abnormality. We’re also looking into types of mammograms that could conform the technology to the actual breast, which would eliminate a lot of the discomfort for patients.”
For ovarian cancer, there are a number of experimental studies and phase one clinical trials underway at HUMC. Not only is the disease notoriously difficult to diagnose, it also doesn’t spread the same way breast or other gynecologic cancers would.

“Ovarian cancers spread in a very unique way,” explained Dr. McNamara. “Because the ovaries hang free in the pelvis, if a tumor develops and ruptures, cancer cells drop into the abdominal cavity. These cancer cells, like seeds, can then spread to the surface of the intestines, surface of the liver, and the outer walls of the uterus, many of which can be microscopic. Therefore, when we discuss a treatment plan, it’s surgically impossible to remove every cancer cell. For this reason, treatment for ovarian cancer virtually always requires a combination of surgery and chemotherapy: surgery to remove tumors that are visible, and chemotherapy to clean up the microscopic residual cells.”
There are several experimental studies in progress for treating ovarian cancer, particularly in immunotherapy, a class of treatments that employs a person’s own immune system to eradicate cancer cells. “For cancer to survive, it has to escape a person’s immune system,” said Dr. McNamara.
“Immunotherapy essentially turns the immune system back on to kill the cancer cells. Patients don’t experience the traditional side effects associated with chemotherapy, like hair loss, nausea, and tingling in the fingers and toes. It’s still under evaluation, but it’s showing great promise.”
Dr. McNamara also highlighted advancements in post-cancer care. Most ovarian cancer is diagnosed in the third stage, and 75% of women who initially respond to treatment will relapse in the future. A novel class of medication, called PARP inhibitors, is oral pills that increase the cure rate of the disease. “Patients can take the medication for up to two years after treatment to help them remain cancer free for longer,” she said.

Of the many technological advances ongoing at HUMC, Dr. McNamara noted one of particular significance is examining tumor biology, which has the potential to increase the effectiveness of cancer treatments across the board. “We send a piece of the tumor to a special lab, located in the cancer center, and they break down the cancer’s DNA, which is different from the DNA of normal cells,” explained Dr. McNamara. “We are looking for specific targets within the genome, and then we can develop drugs that target that specific cancer. It’s exciting stuff.”
Clinical innovation and cutting-edge research are critical in advancing cancer care for her Garden State neighbors, but Dr. McNamara said empathy is an equally important cornerstone of her practice. For her, choosing to specialize in gynecological oncology was personal, as her mother was diagnosed with ovarian cancer when Dr. McNamara was a medical student.

“She was afraid to talk to her oncologist and ask questions, and the oncologist didn’t encourage her,” said the doctor. “I felt I could do a better job. I try to give my patients as much time and empathy as I can so they feel prepared for the journey that lies ahead.”
Compassion is a hallmark of the cancer center at HUMC, where a group of medical and gynecologic oncologists all women work in the same hall, consulting with one another on a daily basis to ensure the best treatment plans for patients. The entire staff, Dr. McNamara noted, takes a team approach to patient comfort. The dietary team offers cooking classes on Fridays, and patients can take part in guided yoga sessions. Social workers are on hand to help guide patients, especially young mothers, through balancing home life with their treatment journey. “We have a wonderful, empathetic team here,” she added.
Hackensack Meridian Health Women’s Oncology
hackensackmeridianhealth.org