AT THE NETWORK WITH THE STATE’S TOP-RANKED UROLOGY PROGRAM, MEN HAVE ACCESS TO THE FULL SPECTRUM OF NEXT-LEVEL PROSTATE CANCER CARE
BY AMANDA McCOY PHOTOS BY AMESSE PHOTOGRAPHY
According to the American Cancer Society, one in eight men will develop prostate cancer in his lifetime, with an estimated 299,000 new diagnoses in 2024 alone. It’s the second most common cancer in men and the number two leading cause of cancer deaths (trailing only skin and lung cancers, respectively). Yet for many, the disease remains shrouded in misconception.

“There’s several reasons men will choose not to get checked for prostate cancer,” explained Michael D. Stifelman, M.D., chair of urology at Hackensack Meridian Hackensack University Medical Center (HUMC) and a global pioneer in robotic urologic oncology. “They might think all prostate
cancers are slow growing or not dangerous, so they assume there is no reason to get screened. But prostate cancer is special; it’s not binary. There are many different types and levels of aggressiveness. Some patients with prostate cancer won’t require any treatment at all, while others with more aggressive cancer will need multi-modality treatment.”
Dr. Stifelman joined Hackensack Meridian Health in 2016, after serving as a full professor of urology at NYU’s School of Medicine for 16 years, where he also ran the robotics program. When he was approached about steering HUMC’s expanding urology program, he was intrigued by the opportunity for growth.
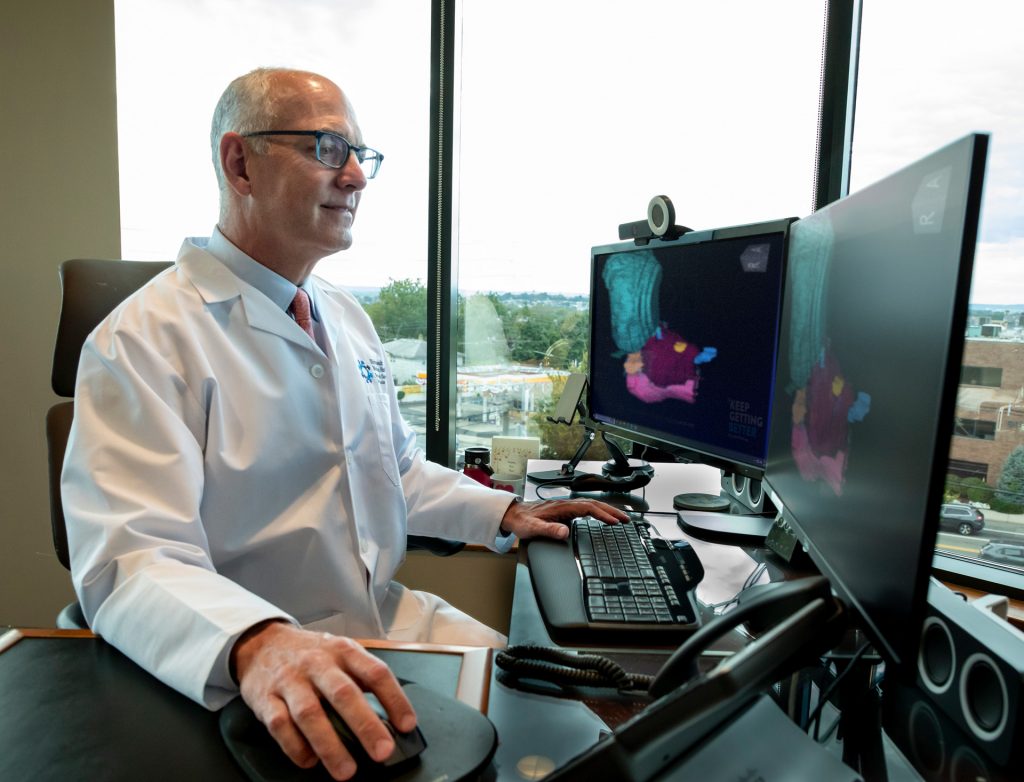
“At Hackensack Meridian Health, there was a larger opportunity for impact,” he noted. “The network is very forward thinking, focused on innovation, quality outcomes, and the best overall experience, not just for the patients but the doctors and staff. I knew there would be an opportunity to innovate and build better, more advanced programs.”
In the eight years since Dr. Stifelman joined Hackensack, the urology program has undergone significant growth. In addition to conducting high-level research and participating in groundbreaking clinical trials, the leaders have brought in a host of cutting-edge technology in robotic surgery, ultrasound, and aquablation therapy. There is now a full residency program in place along with two specialized fellowships. In 2024, HUMC was recognized by U.S. News & World Report as a Top 20 urology program in the country, a proud achievement for Dr. Stifelman and his team.

At HUMC and throughout Hackensack Meridian Health’s hospitals, Dr. Stifelman noted patients have access to the latest in prostate cancer screening tools. The time to discuss screening with your doctor is between ages 55 and 70; however, other factors can increase a person’s risk, including ethnicity, genetic mutations, and family history, when screening may be recommended as early as 40,” added Dr. Stifelman.
Initial screening includes a PSA test, which measures levels of prostate-specific antigen in the blood to determine a patient’s risk of developing prostate cancer.
“If your PSA is less than 1, the risk of you developing prostate cancer is much less than the average population, and you might not need to be screened every year,” explained Dr. Stifelman. “But elevated PSA levels don’t always indicate cancer. Next, we’ll order a confirmatory blood test to assess whether further evaluation is needed, and if so, we conduct the biopsy transperineally using guidance from an MRI, so it’s less painful, more accurate, and has much less risk of infection. It’s our standard of care at Hackensack University Medical Center.”

Like all cancers, prostate cancer is most treatable when detected early, and a significant number of patients won’t require treatment at all. If the cancer is considered low risk, Hackensack Meridian Health physicians might recommend active surveillance, which monitors the tumor through regular test ing. If the cancer is more aggressive, Dr. Stifelman noted the patient has the full gamut of treatment technology available to him, from radiation and cryotherapy to high intensity ultrasound and robotic-assisted surgery.
“Hackensack Meridian Health has always been on the forefront of cutting edge surgery, innovative diagnostics, and best-in-care outcomes,” added Dr. Stifelman. “We’re always looking to do things better. Not only do we offer the full spectrum of care, but we gather all the data possible – through blood markers, genetic testing, MRI, PSA tests, and more to create a personalized treatment plan for each individual patient. It’s not just technology that sets us apart; for every risk category we have at least one active clinical trial available for patients to participate in.”

Looking ahead, Dr. Stifelman said care is going to continue to become more personalized and precise. Deeper research into genetic analysis will help physicians more accurately identify the best treatment course for each individual case, and new treatment options for higher risk patients have the potential to significantly improve both surgical and radiation outcomes. “Hopefully, in my lifetime, we’ll reach a point in medicine where no one will ever die from prostate cancer again,” added Dr. Stifelman.
Hackensack University Medical Center, Urology
hackensackmeridianhealth.org/en/services/urology/elevated-psa
To find a urologist or other health expert at any of the
Hackensack Meridian Health hospitals, call 844-HMH-WELL